Some wisdom teeth erupt normally, but many arrive late and disrupt nearby teeth. They often push at odd angles. This pressure may crowd or shift existing molars. Pain starts subtly. It may feel like pressure near the jaw hinge or lower gums. With time, chewing becomes uncomfortable. Swelling follows. Even if only one tooth causes issues, all four may be affected. Their arrival rarely goes unnoticed for long.
The gums swell slightly at first, then form a flap over the partially emerged tooth
The gums swell slightly at first, then form a flap over the partially emerged tooth. Food gets trapped. Bacteria settle. Infection can follow. The area becomes tender. It hurts to brush. It hurts to eat. Inflammation sets in. This condition, called pericoronitis, often recurs. Antibiotics help, but the tooth remains a risk. Removal becomes not just an option, but a practical solution.
When molars shift due to wisdom teeth, orthodontic results may start to reverse
When molars shift due to wisdom teeth, orthodontic results may start to reverse. Straightened teeth begin crowding again. Braces or aligners can’t hold the line against new pressure. Some patients notice this movement early. Others feel it only when pain arrives. If you’ve had dental correction, your dentist may recommend proactive removal. Not for pain—but to preserve alignment before it’s lost.
Jaw stiffness after waking may be an early sign of impacted wisdom teeth
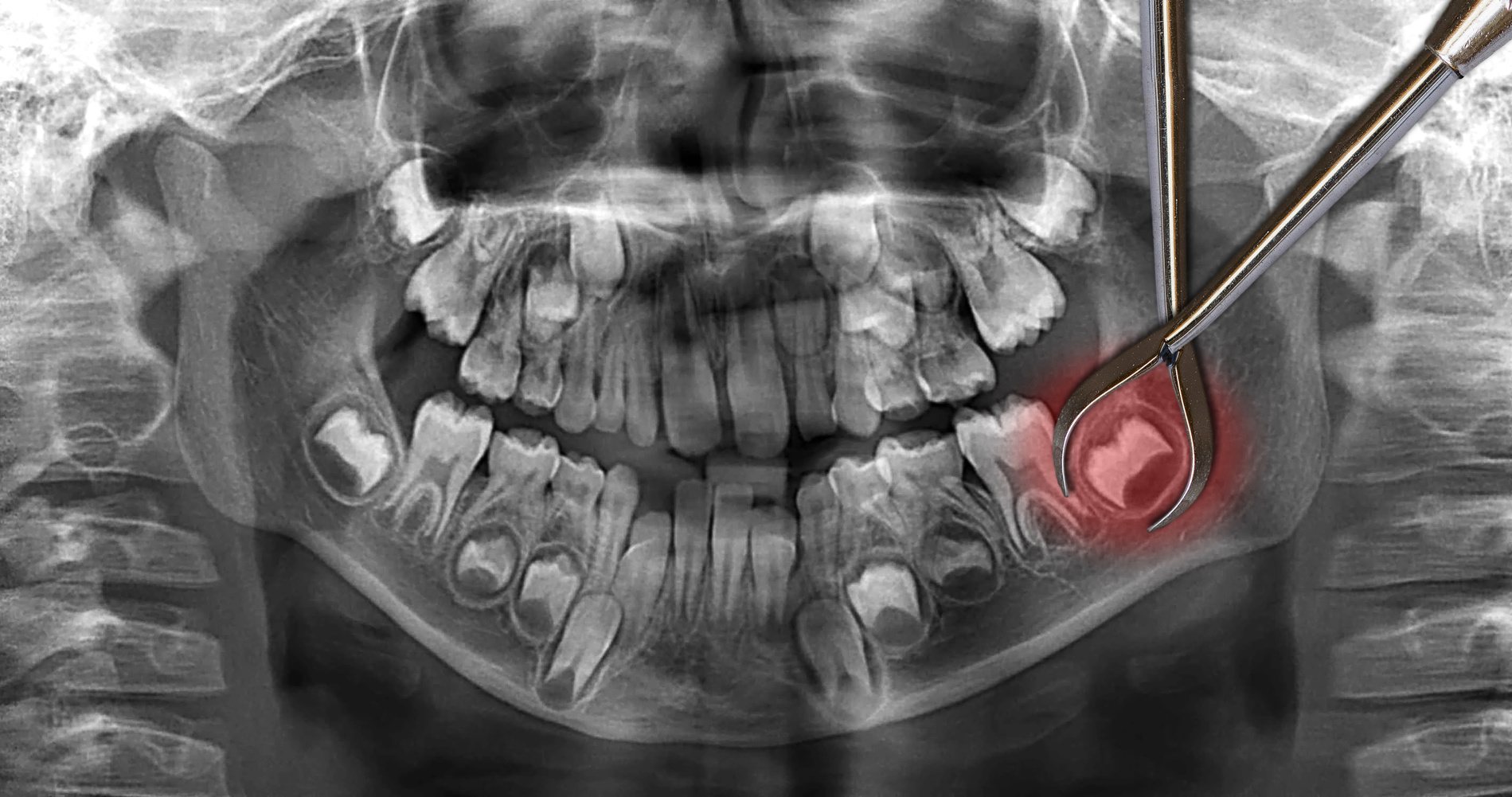
Jaw stiffness after waking may be an early sign of impacted wisdom teeth. The joint aches. Opening wide becomes difficult. The discomfort builds quietly, then sharpens. Impacted teeth press against bone or other roots. They sit sideways or stay buried. Some never erupt. But the body still feels their presence. Imaging often reveals the real position—hidden under gum and pushing inward.
Numbness in the lower lip may indicate nerve compression from a deeply rooted tooth
Numbness in the lower lip may indicate nerve compression from a deeply rooted tooth. Not all wisdom teeth sit high. Some grow near major nerve pathways. As they shift, they touch sensitive branches. This doesn’t always cause pain. Instead, it feels like tingling or loss of sensation. These cases demand careful imaging. Dentists assess risk closely. Removal near nerves requires precision and timing.
Wisdom teeth that decay below the gumline are hard to clean and often stay infected
Wisdom teeth that decay below the gumline are hard to clean and often stay infected. Their angle makes brushing ineffective. Floss doesn’t reach them well. Over time, cavities form. These aren’t small issues. Decay spreads. Infection travels to nearby roots. In some cases, it leads to abscess. Extraction is often easier than managing repeat infection. The longer they stay, the harder the cleanup becomes.
Pain that radiates to the ear or temple may come from pressure in the jaw’s rear
Pain that radiates to the ear or temple may come from pressure in the jaw’s rear. Wisdom teeth don’t always hurt where they sit. The pain refers outward. It mimics headaches or earaches. Some patients chase unrelated causes for months. Only imaging reveals the culprit. A tilted molar pushes bone, not nerves directly. Still, the pain arrives through shared pathways.
Removal becomes urgent when cysts begin forming around impacted teeth
Removal becomes urgent when cysts begin forming around impacted teeth. These cysts grow slowly. But they displace bone, damage roots, and distort alignment. Some remain painless until discovered on scans. Left alone, they risk becoming tumors. Surgery grows more complex as bone erodes. Early removal prevents long-term issues. It isn’t just about comfort—it’s about stopping irreversible changes.
If chewing shifts to one side, it may reflect subconscious avoidance of pressure
If chewing shifts to one side, it may reflect subconscious avoidance of pressure. The body adapts before the mind notices. Jaw imbalance follows. One side overworks. The other weakens. Muscles stiffen unevenly. Dentists spot this pattern during exams. It often links back to a single problematic molar. Realignment after extraction takes time. But balance begins returning once pressure is removed.
Not all wisdom teeth need removal, but those that grow crooked rarely remain quiet
Not all wisdom teeth need removal, but those that grow crooked rarely remain quiet. Some erupt cleanly and fit. Others turn sideways. The angle makes all the difference. Regular checkups help track movement. Dentists monitor spacing, crowding, and gum response. Waiting is only safe when movement stops. If things shift each year, removal is often inevitable. Still, not every case requires action.
Healing after extraction varies by age, position, and root development
Healing after extraction varies by age, position, and root development. Younger patients recover faster. Their roots are softer. The bone fills in smoothly. Older patients take longer. Roots grow deeper and twist. Surgery becomes more invasive. Post-op swelling increases. Dry socket risk rises. Age alone doesn’t dictate removal—but it influences timing. Earlier extraction often means fewer complications later.
Preventive removal is often discussed during the late teens or early twenties
Preventive removal is often discussed during the late teens or early twenties. This timing isn’t random. Roots haven’t fully formed yet. Bones remain flexible. Healing goes quicker. Imaging gives clearer insight. It’s not about rushing surgery—but staying ahead of problems. Some teeth remain silent forever. Others don’t. Early evaluation reveals which direction they’re likely to take.