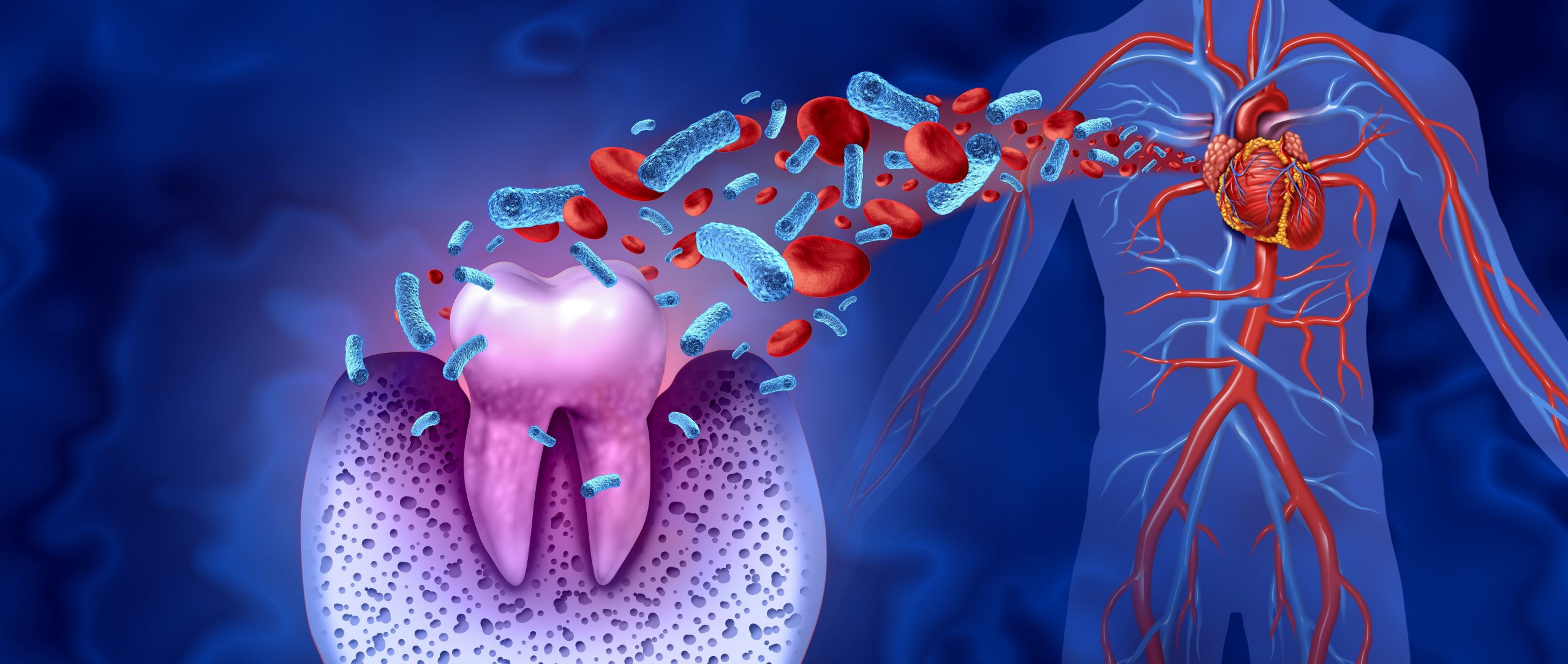
Your mouth hosts hundreds of bacterial species. Most are harmless. Some become harmful when plaque builds. Brushing poorly allows bacteria to thrive along the gums. These bacteria can enter the bloodstream through small tears or inflamed gums. From there, they travel through the body. Bacteria from the mouth can enter the bloodstream—and that’s where the link to the heart begins.
Inflammation in the gums may trigger inflammation in blood vessels
Gum disease doesn’t stay confined to the mouth. Chronic inflammation spreads chemical signals through the body. These inflammatory markers may trigger a similar response in artery walls. Over time, the blood vessels begin to stiffen and thicken. Inflammation in the gums may trigger inflammation in blood vessels—even without other risk factors.
Periodontitis has been linked to increased heart attack risk
Periodontitis is advanced gum disease. It involves bone loss around the teeth. People with periodontitis often show higher levels of systemic inflammation. Studies suggest they face a greater risk of heart attack. The damage doesn’t stop at the jaw. Periodontitis has been linked to increased heart attack risk across diverse age groups.
C-reactive protein levels rise in both gum disease and heart disease
C-reactive protein (CRP) is a marker of inflammation. It’s used to evaluate heart attack risk. People with gum disease often show elevated CRP levels. These levels drop when oral health improves. C-reactive protein levels rise in both gum disease and heart disease, showing a shared biological pathway.
Oral bacteria have been found in heart valve tissue
In patients with heart infections, dental bacteria are sometimes discovered in valve tissue. Streptococcus mutans and other species known for causing cavities have appeared in heart samples. This confirms migration. Oral bacteria have been found in heart valve tissue, suggesting direct involvement in cardiovascular disease.
The same habits that protect the heart benefit the gums
A healthy diet reduces heart risk. It also improves gum health. Smoking harms arteries and weakens the immune defense in the mouth. Stress raises blood pressure and also reduces saliva flow. The same habits that protect the heart benefit the gums—showing why prevention works holistically.
People with diabetes face a double challenge
Diabetes increases the risk of both gum disease and heart disease. Elevated blood sugar damages blood vessels and weakens immune defenses. In the mouth, this leads to slower healing and more severe inflammation. People with diabetes face a double challenge—oral care becomes essential for vascular health.
Missing teeth may reflect more than dental history
Tooth loss doesn’t only affect appearance or chewing. It often signals long-standing gum disease. Researchers have linked tooth loss to higher cardiovascular risk, especially in middle-aged adults. The fewer teeth, the higher the risk. Missing teeth may reflect more than dental history—it may mark systemic health decline.
Bleeding gums aren’t always harmless
Many people see bleeding during brushing and ignore it. They assume they’re brushing too hard. But bleeding gums are a sign of inflammation. That inflammation may indicate underlying disease activity. Bleeding gums aren’t always harmless—they might signal a process that affects more than your smile.
Oral infections can strain the immune system
A chronic oral infection constantly activates the immune system. The body stays alert, expending energy and increasing inflammation. Over time, this low-grade stress affects how the body handles other threats. Oral infections can strain the immune system, creating systemic vulnerability.
Dental neglect increases systemic risk without warning
Some people avoid the dentist for years. Pain brings them back, not prevention. But the mouth can hide damage. Gum disease progresses quietly. Dental neglect increases systemic risk without warning—sometimes the first sign is a cardiac event.
The mouth reveals early signs of chronic inflammation
Dentists often spot chronic disease before physicians do. Dry mouth, gum recession, loose teeth—these aren’t isolated problems. They reflect poor circulation, immune suppression, or ongoing inflammation. The mouth reveals early signs of chronic inflammation, especially in people who seem otherwise healthy.
Brushing and flossing reduce bacteria that affect arteries
Daily brushing removes plaque that hosts bacteria. Flossing clears spaces where inflammation starts. Together, they prevent gum infections. This reduces the number of bacteria entering the bloodstream. Brushing and flossing reduce bacteria that affect arteries—it’s not just cosmetic care.
Heart patients are sometimes prescribed antibiotics before dental procedures
People with valve problems or past infections may take antibiotics before cleanings. This reduces the risk of bacteria spreading. It’s not needed for everyone. But it shows medical acknowledgment of the mouth–heart connection. Heart patients are sometimes prescribed antibiotics before dental procedures—highlighting the serious crossover between fields.
Dental cleanings can lower systemic inflammation levels
Studies show that people with gum disease who receive deep cleanings experience a drop in inflammatory markers. Not just in the mouth—but across the whole body. Dental cleanings can lower systemic inflammation levels, even when patients feel no symptoms.
Gum disease treatment improves blood vessel flexibility
Healthy arteries expand and contract with ease. Inflammation stiffens them. After gum treatment, some patients show improved vascular response. Their blood vessels function better. Gum disease treatment improves blood vessel flexibility—a measurable cardiovascular benefit from oral care.
Mouth bacteria contribute to plaque buildup in arteries
Atherosclerosis involves fatty plaques narrowing the arteries. Some of this plaque includes bacteria. DNA testing has traced these bacteria to oral origins. Mouth bacteria contribute to plaque buildup in arteries, increasing the chance of heart attack or stroke.
Flossing may help lower your heart disease risk
Flossing isn’t just about fresh breath. It removes bacteria that cause gum inflammation. That same inflammation may travel beyond the jaw. Flossing may help lower your heart disease risk—one simple step that affects multiple systems.
People with heart disease should inform their dentist
Medical history affects dental planning. Certain heart medications cause dry mouth. Others increase bleeding risk. Some require pre-procedure adjustments. People with heart disease should inform their dentist—not just for safety, but for integrated care.
Integrated care between cardiologists and dentists is still rare
Most patients see these doctors separately. Records aren’t shared. Symptoms are considered in isolation. But the science supports collaboration. Integrated care between cardiologists and dentists is still rare—though it may become necessary as research grows.