Some people want a permanent solution after years of living with removable dentures. Dentures can become loose, irritate the gums, and shift during meals. Many patients feel uncomfortable speaking in public because of fear they might move. While dentures improve appearance and chewing, they do not stop jawbone loss. Over time, this leads to facial structure changes and discomfort. Dental implants address both function and bone support. They offer a fixed option that feels closer to natural teeth. For individuals seeking long-term stability, implants become a serious consideration. The transition isn’t immediate, but the difference can be lasting.
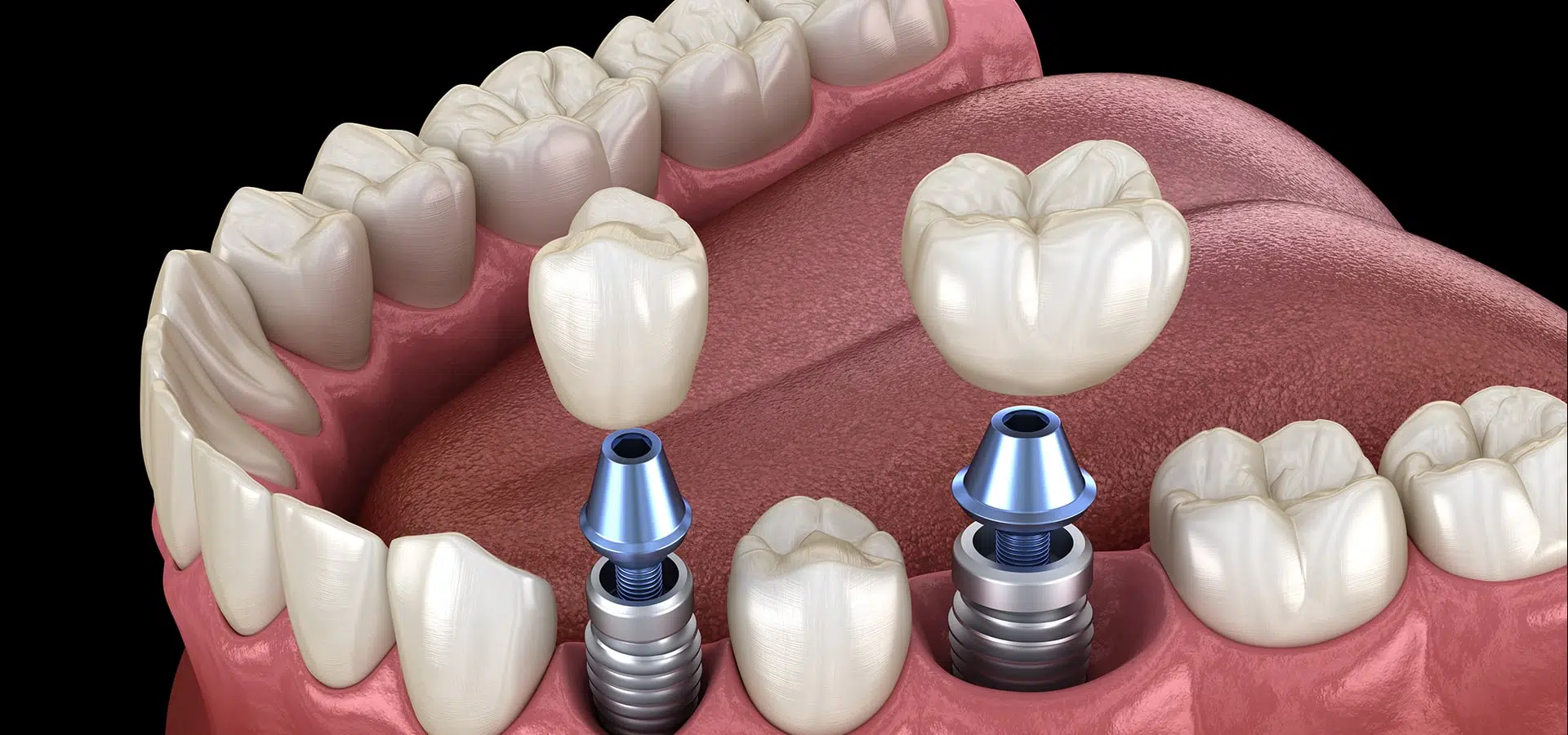
Dental implants involve inserting a titanium post directly into the jawbone
Dental implants involve inserting a titanium post directly into the jawbone. This post acts like a root. After insertion, the surrounding bone gradually fuses with the metal through a process called osseointegration. Once healed, a crown is attached to complete the tooth replacement. This integration provides strong support that mimics a natural tooth. It also helps preserve bone structure, which regular dentures cannot achieve. The timeline varies—some need months of healing, others follow same-day protocols. Not all patients are eligible immediately. Bone density and gum health influence success rates and determine readiness.
Bone loss in the jaw can affect whether you’re a good candidate for implants
Bone loss in the jaw can affect whether you’re a good candidate for implants. When teeth are missing for a long time, the bone in that area starts to shrink. Without enough volume, the implant cannot anchor properly. In such cases, bone grafting might be necessary. This process adds material to rebuild volume where it’s lacking. Healing time adds months to the timeline, but it increases long-term success. Dentists evaluate bone through X-rays or 3D scans before deciding on the procedure. If grafting isn’t an option, alternative treatments may be suggested. The structure must support the implant safely.
People with uncontrolled diabetes or heavy smoking habits may face lower implant success rates
People with uncontrolled diabetes or heavy smoking habits may face lower implant success rates. Healing relies on strong circulation and immune support. Smoking reduces blood flow and introduces toxins that interfere with tissue repair. Similarly, poorly managed diabetes delays healing and increases infection risk. Some people can still get implants if their condition is well controlled. Dentists assess medical history closely and may collaborate with other doctors. The implant procedure is elective but invasive. Patients need to understand both benefits and risks. A healthy foundation improves both integration and longevity of the implant.
Implants require commitment to long-term oral hygiene and regular dental visits
Implants require commitment to long-term oral hygiene and regular dental visits. Unlike natural teeth, implants don’t decay. But the surrounding tissue remains vulnerable to inflammation. Peri-implantitis is a condition where plaque builds up around the implant, threatening its stability. Brushing and flossing must be consistent. Special tools like interdental brushes or water flossers may help. Routine dental cleanings ensure early detection of issues. Implant care involves the same attention as natural teeth—sometimes more. Neglect leads to failure, despite good surgical placement. A successful implant begins with surgery but survives through daily maintenance.
Some patients report that implants feel more natural than any other dental solution they’ve tried
Some patients report that implants feel more natural than any other dental solution they’ve tried. They don’t move during meals or speech. Chewing becomes easier, especially with crunchy or sticky foods. Unlike dentures, implants do not press on the gums. That reduction in pressure can decrease pain and ulcers. The confidence of biting without hesitation improves quality of life. Patients often stop thinking about the tooth altogether, which rarely happens with removable options. This sense of normalcy is what many people value most. It doesn’t appear immediately but grows with time and adaptation.
The upfront cost is higher than other options, but many see it as a long-term investment
The upfront cost is higher than other options, but many see it as a long-term investment. Dentures or bridges may need replacing more frequently. Implants, when maintained well, can last decades. While insurance coverage varies, payment plans or staged treatment help reduce financial pressure. The cost includes not only the implant but also scans, surgery, and follow-up care. Price should be weighed against expected durability. For some, affordability is a barrier. Others decide based on lifestyle, comfort, or previous dental failures. The financial conversation is part of the consultation and rarely avoided.
Healing varies widely and influences how soon the final tooth can be placed
Healing varies widely and influences how soon the final tooth can be placed. Some patients need months before full integration. Others qualify for immediate loading protocols. Healing depends on bone quality, surgical precision, and immune health. Swelling, minor discomfort, and diet restrictions are normal during recovery. Regular check-ups track progress and spot complications early. Patients who rush back into normal habits sometimes delay healing. Understanding that implants are a process, not an event, makes the journey easier. The timing may feel slow, but it ensures stronger outcomes. Patience is part of the treatment plan.
Not every missing tooth needs an implant—sometimes fewer implants support larger restorations
Not every missing tooth needs an implant—sometimes fewer implants support larger restorations. For example, full-arch prosthetics can be anchored by as few as four implants. This method reduces cost and surgical time while offering full function. Some patients opt for implant-supported bridges instead of individual implants. This approach suits cases where adjacent teeth are also missing or damaged. The decision depends on spacing, bite force, and gum condition. Dentists explain these configurations clearly during evaluation. The number of implants is based on support needs, not simply the count of missing teeth.
Choosing implants is personal and shaped by comfort, health status, and life goals
Choosing implants is personal and shaped by comfort, health status, and life goals. Some people want freedom from adhesives. Others want to preserve bone. Some avoid surgery altogether. Age, health conditions, and financial priorities all influence the decision. Dentists help clarify what to expect, but the choice remains with the patient. Implants are not the only solution—but they offer unique advantages. Every decision begins with honest reflection. The right choice is not universal. It’s specific, and it starts with asking the right questions.